Why we must give terminally ill patients choice
This week, parliament will be confronting two issues of life and death: an end to the criminalisation of abortion which takes place outside the currently permitted time periods; and the introduction of a - highly qualified - right to assisted dying for those who are terminally ill.
In both cases, there is a mix of fundamental principle around the meaning and value of life and practical, legislative detail. Both subjects arouse strong emotions. And both debates show parliament at its best, transcending the petty, tribal, party-political banter, which is what the public so often sees.
I have followed the assisted dying issue with particular interest since I came very high in the ballot for Private Members legislation in the 2017-19 parliament and was about to introduce a Bill to legalise assisted dying when the ‘Brexit election’ intervened (in truth, the composition of parliament then meant that it was unlikely to pass).
I felt conflicting emotions and saw the strength of arguments on both sides. I had, moreover, changed my mind from being hostile to becoming an advocate of assisted dying.
Like many MPs, then and now, my judgements were informed by personal experience. My mother died in her mid-80s in a state of mental confusion and also of depression, worried about being a burden. Under excessively permissive legislation she could easily have been talked into signing away her life.

My late wife died of terminal cancer in her mid-50s when she had so much more to give and to enjoy. She had a strong and courageous personality and made it clear that she did not wish to terminate her life and wished to die at home surrounded by a loving family and with palliative support.
These two experiences helped form my view that assisted dying was potentially dangerous and unnecessary. But my views evolved when, as an MP, I encountered people who faced an undignified and painful end to their lives and wished to have some agency over it. They were fully lucid and unambiguous that they wanted help to die. But the law forbade it.
There were terminally ill cancer patients who felt that they had lived their lives and wanted to be spared the last few weeks of suffering. And there were patients in the advanced stages of Motor Neurone Disease (MND) who were losing all control of their bodies while retaining clear awareness of what was happening to them. Meeting and talking to such people was deeply humbling and forced me to reappraise the arguments.
But good cases can make bad law. It has long been clear that there must be strong safeguards: to prevent people committing to assisted dying because they feel themselves to be a burden; or feel under pressure from relatives eying an inheritance; or are passing through temporary depression (like my mother); or simply lack access to the pain relief or other palliative care which could make the end of life more tolerable.
The legislation passing through the Commons this week contains strong safeguards in the form of a need to obtain the approval of two doctors and a three-person panel. Moreover, the right to assisted dying is restricted to the terminally ill with a medical diagnosis of six months life expectancy (which will have the effect of excluding many MND cases where life expectancy is difficult to measure).
Even then, many doctors fear that life will be cheapened and that the safeguards will be insufficient. The Royal College of Psychiatrists opposes the Bill fearing that mental illness could blur patients’ judgements. Others point to seemingly miraculous cures or to people like the physicist Stephen Hawking who lived with MND for over 50 years after his diagnosis and made a massive contribution to learning.
Others have argued that good palliative care is an alternative to assisted dying for many patients (as my late wife demonstrated). My successor as MP for Twickenham, Munira Wilson, has secured an important amendment requiring regular reporting on the availability of palliative care.
Another necessary protection is for doctors and nurses who have religious or wider ethical concerns about assisted dying. They will not be obliged to participate in any assisted dying cases.
Many MPs who still feel undecided want delay for further reflection or to gather more evidence. There is however plenty of experience to draw on from countries like Canada which have been down this road. And, even if the legislation passes, nothing will happen quickly. It will take another two years before the Bill completes its passage through parliament and Royal Assent to the new law is obtained; and then another two years before the law comes into effect and longer still for an assisted dying service to become operational.
This issue potentially affects all of us. Now in my 80s, I see more and more friends and acquaintances dying. Many are said to have had ‘a good death’. Others, almost certainly, did not. I am fortunate to have managed to stay largely free of the diseases of old age and to enjoy a busy, physically and mentally active and fulfilling life. But at some point, age will catch up with me. I would then like to feel that I have some control over what happens next.
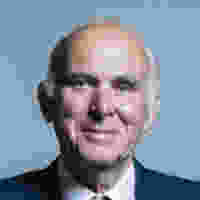
Sir Vince Cable is a former Secretary of State for Business, and led the Liberal Democrats from 2017-19.