The threat of disposable PPE must be addressed
Face masks have been an important infection prevention tool in medical settings since the 19th century. Tragically these products, designed to limit the spread of disease, are now having a devastating environmental impact—and risk causing new infectious outbreaks exacerbating the “Grand Pandemic” of antimicrobial resistance (AMR).
Recent decades have seen a massive proliferation in the use of disposable plastic-based personal protective equipment (PPE), which has become standard procedure in medical settings. As many as a billion face masks are distributed in the NHS for use every year and; staggeringly, the majority of these are not recycled. During COVID-19 pandemic community masking became a worldwide infection prevention strategy as never seen before, further increasing demand and production of face masks.
Environmental contamination from PPE is creating novel health threats
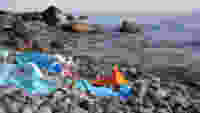
Beyond driving shortages of critically needed medical PPE, the widespread increase in the use of face masks is of deep environmental concern. Face masks scattered as litter became an all too common sight, from our local parks and roads to our oceans and waterways. It is essential that progress be made to reduce the environmental impact and improve the sustainability of PPE, considering its lifecycle from production to disposal.
The very fibres of medical and community face masks are well known to be a source of plastic and microplastic pollution in the environment. An undeniable body of evidence highlights that a significant amount of PPE makes its way into aquatic environments, contributing to the pre-existing plastic pollution and posing further serious risk of infectious disease. This latter point was, until recently, deeply underexplored. However, there is now solid evidence showing that microplastics in water and soil can act as vectors for both pathogens themselves and the genes associated with antimicrobial resistance. Emily Stevenson, a previous intern in my Office funded by the British Society for Antimicrobial Chemotherapy (BSAC), has recently published an excellent review of this topic.
It is estimated that trillions of microplastic particles now contaminate our oceans; our health protection equipment can’t continue to contribute to this. This is stark reminder that the indivisible climate and nature crises are a global health emergency and need to be treated as such, as has been called for by over 200 health journals. We must empower research and development to provide solutions, offering alternative fabrics which do not rely on harmful polymer fibres (e.g. applying green chemistry to develop novel degradable polymers or using biodegradable materials), and to move away from a ‘single use system’ as the standard in healthcare settings.

The UK is moving too slowly
This year the government has been trialling use of washable PPE, with estimates that replacing disposable PPE with reusable PPE could save £180 million a year. However, given the well documented release of microplastics from synthetic fabrics during washing, biodegradable materials which do not leach plastic and microplastic into the environment are still needed for sustainability. Other reuse systems could provide PPE cleaning with novel methods such as UV radiation to avoid plastic pollution entering water systems. It is important to develop the evidence base, which his currently lacking, for alternative cleaning methods. Given the substantial potential benefits, we need to move quickly to ensure policies are in place to support the transition to reusable PPE in healthcare. As I raised during the House of Lords debate on washable PPE earlier this year, this also requires investment in infrastructure to ensure hospitals are equipped with laundry or other facilities necessary to facilitate PPE washing.
As much of a threat as plastic pollution is, it is not the only concern for our health or the exacerbation of AMR. Commercially available face masks are permitted to contain antimicrobial agents as a selling point, including a variety of metal-based nanoparticles. This is particularly worrisome in the case of silver nanoparticles, a popular choice due to their broad-ranging antimicrobial activity. Until fairly recently it was mistakenly accepted that bacteria could not develop resistance to the complex antimicrobial action of nanoparticles (and silver in general). A growing body of evidence has now revealed that the widespread use of silver compounds has in fact led to the evolution of silver-resistant bacteria. Indeed, research has highlighted a terrifying further emerging-phenomenon of metal-driven co-selection of antimicrobial resistance, whereby the same genes grant resistance to both heavy metals and antibiotics, putting our already limited pool of drugs at further risk.
Biocidal compounds should not be used without proper examination of the risks
The use of silver in face masks is not only an environmental concern, but also presents a unique personal risk, due to the possibility particles being ingested by the wearer which may negatively impact the microbiome and could, in the case of infection, drive antimicrobial resistance by co-selection. Researchers have indeed already highlighted this risk and demonstrated using bespoke experiments that several masks that are commercially available for the general public do indeed cross the safety limit values for current inhalation exposure to silver ions and silver nanoparticles.
To reduce the development and impact of silver resistance, there are two main challenges. Firstly, it is crucial that further research be conducted into the safety of face masks containing antimicrobial compounds, in particular heavy metal nanoparticles. Currently we do not have standards for testing exposure to nanoparticles during mask wearing and research is limited by a lack of consistency in safety testing during development. Secondly, policy and regulation must be in place to ensure product safety and informed decision making for both healthcare procurers and the general public. The use of silver nanoparticles in biocides was banned under EU regulation in 2021, however this does not extend to their use in fabrics for face masks with some researchers calling for tighter regulation. I have twice submitted a Private Member’s Bill which would have seen biocides banned from use in consumer products in the UK. We must increase awareness and support to enact the necessary changes to address this critical and unnecessary risk to health.
The aim is not to stifle innovation; in fact appropriate use of antimicrobials in face masks may provide novel routes to increasing the effectiveness of face masks in preventing spread of infection, while also increasing their lifetime and reusability. As highlighted in a review by my current BSAC Parliamentary intern Katy Stokes, studies have shown promising results in this direction. However, it is crucial to ensure the safety and regulatory standards are in place to support such innovations. The government must support the NHS in transitioning to more sustainable PPE options and also foster the research underlying their use.
This article was written with the assistance of Katy Stokes, a British Society for Antimicrobial Chemotherapy-funded Parliamentary Intern
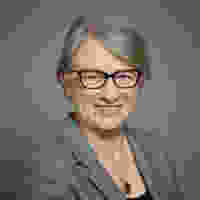
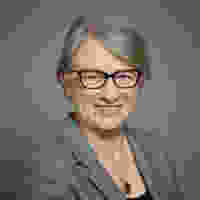
Baroness Natalie Bennett is a member of the House of Lords and led the Green Party from 2012-2016.