Let's empower community pharmacists on antibiotics
On the face of it, new plans announced by the Government to give community pharmacists the ability to prescribe patients antibiotics, for some conditions, without a prescription from their GP could be very beneficial. But has the Government made a careful enough assessment of the long-term consequences of this policy, and the resources needed to implement it?
Its objective is to end the ‘8am scramble’ for GP appointments, reduce the workload of already stretched GPs and drive down waiting times. Empowering community pharmacies to this end could improve access to care, especially in more deprived areas. However, without increased funding for staffing, training and point of care diagnostics, this rollout could lead to severe consequences, including potential increases in antimicrobial resistance (AMR).
That’s an issue that’s taking up a lot of my time, from taking part in the ABX Network (representing researchers hunting for potential new antibiotics), gathering in Norwich, to hosting the launch of the Action for Animal Health’s report The case for investing in animal health to support One Health, to speaking on the issue, as part of a broader focus on the risks from exceeding the planet’s capacity to deal with “novel entities”, at the International Festival of Public Health in Manchester. Activities in the area are stepping up in advance of the expected renewal of the UK’s national action plan for dealing with AMR.
Bacterial infections continue to be a major source of mortality across the world, with one in eight deaths now linked to these infections. AMR claims as many lives in the UK as breast cancer each year, yet gets far less attention, while of antibiotic resistance are still increasing year on year across the country and globally.

There’s also great concern about the pressure on pharmacies, as all other parts of our healthcare system, and, as Bristol Councillor Carla Denyer drew to my attention, worries that assessment of provision takes into account the total number and location of pharmacies, but not their opening hours and quality and breadth of provision, which can leave particularly the most disadvantaged communities, with the greatest needs, under-serviced. (I’m asking the government a written question about that now.)
The plans set out by the government would allow for pharmacists to prescribe antibiotics for the following seven conditions: earache, sore throat, sinusitis, impetigo, shingles, infected insect bites and uncomplicated urinary tract infections (UTIs). However sore throats and ear infections, for example, are more often caused by viruses such as the common cold or flu, rather than bacterial infections. There is therefore no medical benefit to prescribing antibiotics, which kill bacteria, to treat infections by these viruses.
Shingles is another example or a viral infection, which can be caused due to the reactivation of the chicken pox virus. These conditions would not require antibiotic treatment, and widespread inappropriate use of antibiotics for these infections could lead to increases in antimicrobial resistance.
One of the key ways that this risk could be minimised would be through improvements to diagnostic testing, particularly for significant pathogens such as Group A Streptococcus (GAS), a well-publicised cause of sore throats, and for UTIs.
A surge in the prescribing of antibiotics for GAS infections in 2022 led to shortages of antibiotics, particularly penicillin. This caused issues for pharmacies, which had to then prescribe more costly alternatives and for patients who needed treatment, particularly those on prolonged antibiotic courses. This policy, absent mitigation measures, could lead to shortages becoming more frequent.
The treatment of uncomplicated UTIs may also be problematic. Determining the types of infection - complicated, uncomplicated or recurrent - can be difficult without full access to patient medical records and diagnostic tests. Urine dipsticks are often used as a point-of-care test to indicate infection. However, these become more unreliable as a patient ages and are not recommended in the over 65s, the patient group most susceptible to UTIs. Further development in these point-of care tests would need to be done to reduce unnecessary antibiotic usage and inappropriate prescribing.
On the other side of the argument, UTIs predominantly affect women, with 50% of women suffering from a UTI at least once in their life. and the ability to receive antibiotics more quickly may improve outcomes. This may be a first step in addressing the poorer healthcare that women receive in the UK compared to men. Another key area that would have to be improved would be training in prescribing for pharmacists.
Inevitably, more trained community pharmacists will be required to cope with the increased demand for over-the-counter antibiotics. In light of the large number of community chemists that have been closing, including 670 pharmacies since 2015 and 160 closing in the past two years, this could prove challenging. As is so often the case, the Government does not appear to have a “joined-up” strategy: no plan to reach the number of trained pharmacists needed to cope with the prescribing increases has been put forward.
There have been discussions for prescribing to be embedded into pharmacy degree programs rather than the current method of achieving a separate postgraduate certificate. Of course, these changes to degree programmes would require additional funding for both training and supporting work placements.
We all want shorter waiting times and less GP burnout from workload. Empowering community pharmacists could be an effective way of achieving this. However, these changes need to be seen as part of a long-term strategy, not a short-term fix. The Government should carefully consider the impacts on AMR and how it intends to fund the necessary training to avoid catastrophic side-effects.
This article was prepared with the assistance of Dr Eleanor Senior
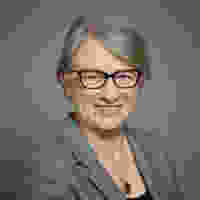
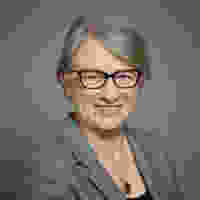
Baroness Natalie Bennett is a member of the House of Lords and led the Green Party from 2012-2016.