We should have the right to end our lives in dignity
Have you ever experienced someone say to you: 'I want to die.'? I cannot remember how many times I have heard these words, and I imagine most nurses working in the NHS will have had a similar experience at least once during their career. My memories of these moments are marked by a profound sadness. As a nurse my first instinct is to preserve life, not help end it.
Sometimes, when you dig deeper into a person’s circumstance, you realise what they actually mean is ‘I want to live, but not like this’. Perhaps the care they are receiving is inadequate, or their pain isn't being managed properly. In those cases, I try my best to find a solution with them and the wider multi-disciplinary team, towards a life they feel is worth living. Other times I must concede that there is nothing within my power, or that of a doctor or palliative nurse, that can change their mind. They've simply had enough.
In these moments I find myself wishing that assisted dying was legal in the United Kingdom. The Parliamentary Office for Science and Technology defines assisted dying as 'the involvement of healthcare professionals in the provision of lethal drugs intended to end a patient's life at their voluntary request, subject to eligibility criteria and safeguards.' Currently, assisting someone to die carries a maximum sentence of 14 years in prison if convicted.
I believe that we as humans have a right to life, as well as the right to end our lives in dignity, when we are either terminally ill, or incurably suffering. The NMC code enshrines our duty as nurses to 'treat people as individuals and uphold their dignity' by meeting them 'with kindness, respect and compassion'. To me, supporting patients in this way would constitute the highest form of respect and compassion. It means taking their request seriously, and acknowledging when prolonging life is no longer the kindest thing to do.
On average, one person a week travels from the UK to Switzerland to seek medical assistance in dying. This option discriminates against those who cannot afford the average cost of around £10,000 GBP, as well as those who physically aren’t able to make the journey. It strikes me that we should not be outsourcing compassion to other countries.

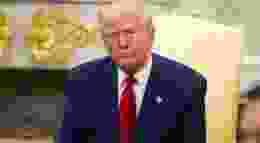
Legislation towards making assisted dying legal is underway in Scotland, Jersey and the Isle of Man, putting pressure on the UK government to review the law. The UK Health and Social Care Select Committee is conducting an inquiry into the subject, meaning that parliamentarians are looking at the evidence from countries such as Canada, Australia, Belgium, the Netherlands and Switzerland, who have had assisted dying laws for many years now. The committee is also asking for the views of people who would be affected by this legislation, campaigners, and healthcare professionals.
As the largest professional group in the NHS, nurses should have their voices heard on this matter. Whether you agree with me or not, nurses are often the ones at a patient’s bedside when a request for an assisted death is made. Our views should be reflected in any proposed legislation, and nurses will have valuable insights into how a law can be designed in the safest, most compassionate way.
I acknowledge the wide range of different opinions on the matter. From the cautious voices within the palliative care community to those living with a disability who are fearful of what a law could mean for them - I hear you. In fact, I want to hear more from you. I want a lively debate about how we can ensure the UK has the strongest safeguards possible, whilst allowing those of sound mind with a terminal diagnosis, or whose suffering has become unbearable, to exercise the right to end their lives.
More than 80% of the UK public support a change in the law. To me, it is a question of when, not if assisted dying becomes legal in the United Kingdom. As nurses, we should ensure our voices are being heard.

Carmen Sumadiwiria is a Specialist Clinical Nurse and is Director of Diversity at My Death, My Decision.